Most frequent infections in patients with Systemic Lupus Erythematosus admitted to the Medical Clinic Service of the Hospital Nacional
Main Article Content
Abstract
Introduction: systemic lupus erythematosus (SLE) is known as a multisystem autoimmune disease, whose cause is unknown, and is characterized by the presence of immune complexes and autoantibodies. In international series, presentation of infectious processes is described in these patients in up to 75 % of cases. Infections occur both at the beginning of the disease and in late stages, and are a direct cause of death in 30 % to 60 % of patients. Cases and reason for hospitalization up to 30 %.
Objectives: determine the most frequent infectious processes in patients with systemic lupus erythematosus admitted to the Medical Clinic Service of the Hospital Nacional in the period 2022-2023.
Methodology: observational, descriptive cross-sectional design of patients with a diagnosis of systemic lupus erythematosus according to criteria of European League Against Rheumatism (EULAR)-2019 who are admitted to the Medical Clinic service of the Hospital Nacional (ItauguáParaguay) in the period of 2022-2023.
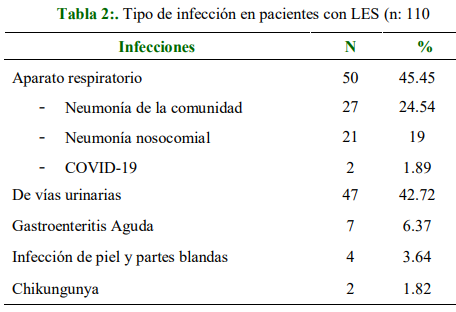
Results: the average age of the patients was 34 years, with a predominance of the female sex in 88.18 %. Respiratory system infections were the most frequently diagnosed in 50 (45.45 %) patients, followed by urinary tract infection in 47 (42.38 %) patients. The predominant risk factor was the use of corticosteroids in a total of 105 (96.40 %) patients, it was established in a total of 97 (88.18 %) patients with antibiotic therapy, within the demographic aspect of the urban area 56 (50.90 %) patients and rural 54 (49.1 %).
Conclusion: respiratory tract infection was the most frequent infection, the predominant risk factor is the use of corticosteroids and they received antibiotic therapy, which in monotherapy was the most used.
Article Details

This work is licensed under a Creative Commons Attribution 4.0 International License.
Usted es libre de:
- Compartir: copiar y redistribuir el material en cualquier medio o formato para cualquier propósito, incluso comercialmente.
- Adaptar: remezclar, transformar y construir a partir del material para cualquier propósito, incluso comercialmente.
- La licenciante no puede revocar estas libertades en tanto usted siga los términos de la licencia
Bajo los siguientes términos:
- Atribución: Usted debe dar crédito de manera adecuada, brindar un enlace a la licencia, e indicar si se han realizado cambios. Puede hacerlo en cualquier forma razonable, pero no de forma tal que sugiera que usted o su uso tienen el apoyo de la licenciante.
- Compartir igual: — Si remezcla, transforma o crea a partir del material, debe distribuir su contribución bajo la misma licencia del original.
- No hay restricciones adicionales — No puede aplicar términos legales ni medidas tecnológicas que restrinjan legalmente a otras a hacer cualquier uso permitido por la licencia.
References
Acosta Colmán I, Avila G, Acosta ME, Aquino A, Centurión O, Duarte M. Clinical and laboratory manifstations in systemic lupus erythematosus. Mem Inst Investig Cienc Salud. 2016;14(1):94–104. Disponible en: http://scielo.iics.una.py/pdf/iics/v14n1/v14n1a14.pdf
Melgarejo Paniagua PA, Denis Doldán AE, Ferreira Gaona MI, Díaz Reissner CV. Complicaciones en pacientes con lupus eritematoso sistémico. Rev. Nac. (Itauguá). 2015;7(2):15-19. doi:10.18004/rdn2015.0007.02.015-019
Enberg GM, Kahn ChM, Goity FC, Villalón SMV, Zamorano RJ, Figueroa EF. Infecciones en pacientes con lupus eritematoso sistémico. Rev Med Chil. 2009;137(10):1367–74. Disponible en: https://www.scielo.cl/pdf/rmc/v137n10/art14.pdf
Crow MK. Etiology and pathogenesis of systemic lupus erythematosus. En: Firestein GS, Budd RC, Gabriel SE, Koretzky GA, McInnes IB, O'Dell JR, eds. Firestein & Kelley's Textbook of Rheumatology. 11th ed. Philadelphia, PA: Elsevier; 2021.
Timlin H, Syed A, Haque U, Adler B, Law G, Machireddy K, et al. Fiebres en pacientes adultos con lupus. Cureus 2018;10(1):e2098. doi: 10.7759/cureus.2098
Serra-García L, Barba PJ, Morgado-Carrasco D. FR-Criterios de clasificación 2019 del lupus eritematoso sistémico. ACTAS Demo-Sifiliográficas. 2022;113:310-312. Disponible en: https://www.actasdermo.org./es-pdf-S0001731021003720
Fanouriakis A, Kostopoulou M, Alunno A, Aringer M, Bajema I, Boletis JN, et al. 2019 update of the EULAR recommendations for the management of systemic lupus erythematosus. Ann Rheum Dis. 2019;78(6):736-745. doi: 10.1136/annrheumdis-2019-215089.
Aringer M, Costenbader K, Daikh D, Brinks R, Mosca M, Ramsey-Goldman R, et al. 2019 European league against rheumatism/American College of Rheumatology classification criteria for systemic lupus erythematosus. Arthritis Rheumatol. 2019;71(9):1400–1412. doi: 10.1002/art.40930.
Urizar C, Troche N, Portillo C. Vista de Frecuencia de complicaciones infecciosas en pacientes con lupus eritematoso sistémico y artritis reumatoide de la III Cátedra de Clínica Médica (2014-2016). Revista Paraguaya de Reumatología. 2016;2(2):2413-4341. Disponible en: https://www.revista.spr.org.py/index.php/spr/article/view/39/84
Noriega-Zapata EJ, Ugarte Gil MF, Pimentel Quiroz VR, Gamboa Cárdenas RV, Reátegui Sokolova C, Alfaro Lozano JL, et al. Factores asociados a infecciones serias en pacientes hospitalizados con lupus eritematoso sistémico. An Fac Med. 2022;83(1):25-33. Disponible en: http://www.scielo.org.pe/pdf/afm/v83n1/1025-5583-afm-83-01-00025.pdf
Ayala Saucedo AR, Torres de Taboada E, Montiel de Jarolín D. Causas de fiebre en pacientes adultos con lupus eritematoso sistémico. Rev virtual Soc Parag Med Int. 2017:4(1):35-45. doi:10.18004/rvspmi/2312-3893/2017.04(01)35-045.
Montiel D, Cacace P. Mortalidad y causas de muerte en pacientes con lupus eritematoso sistémico 2019. Rev. parag. reumatol. 2019;5(2):51-57. doi: 10.18004/rpr/2019.05.02.51-57.
Torres Boggino E, Taboada V, Montiel D, Velázquez G. Factores de riesgo de hospitalización y mortalidad de pacientes internados con lupus eritematoso sistémico en Paraguay. Rev. cient. salud. 2023;5:e5118. doi: 10.53732/rccsalud/2023.e5118.